Failed IVF is a frustrating situation for couples and their fertility doctors.
There is an equation that we can use to illustrate the implantation process:
- Embryo quality + receptivity of uterine lining = chance for implantation and pregnancy
- We know that many human embryos will arrest (die) before day 5
- Unfortunately, embryonic arrest also occurs after day 5
- Some of the embryos that we transfer that “look good” will die after we put them in the uterus
- This is the explanation for IVF failure in the large majority of cases
- The problem is rarely the sperm, and uncommonly the uterus
- It is usually a weakness in the embryo that leads to failed implantation
- On the average, only about 25% of transferred embryos continue to develop and become kids
- This percentage of implanting embryos is greatly dependent on female age
- We see about 50% implant under age 35
- We see about 12% implant at age 41-42
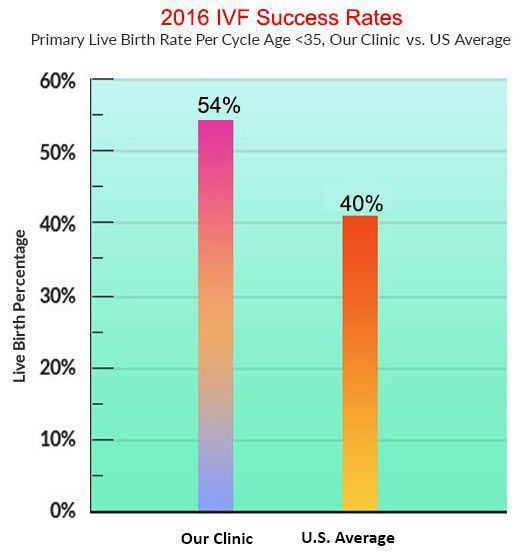
Our success vs. national average
Data from 2016 SART report
Patients that fail IVF will often ask...
- “Why didn’t the embryos stick, did you put them in the right spot?”
- “What’s wrong with my uterus – it’s not accepting the embryos?”
Sometimes, after repeated failure to implant any embryos with IVF, women will say;
- “Obviously, I need a surrogate to carry the embryos because my uterus can’t do the job”.
Although this could be logical. It does not fit with the science. When IVF does not work after numerous attempts – switching the uterus is not likely to result in success. However, the egg donation experience teaches us that switching to eggs from a young egg donor would be very likely to be successful.
This tells us that the problem is not the uterus but is the egg quality. Therefore, it works when we switch to different eggs from a young woman.
Some animal species have much higher implantation rates per embryo transferred than humans do. Human IVF is not as efficient due to the relative weakness of the human egg as compared to those animal species.
This is not to say that the sperm and the uterus are not sometimes contributing factors in the IVF success equation. However, the sperm and the uterus are relatively minor factors as compared to the major factor of egg quality.
Genetic and chromosomal issues causing causing failure of implantation in IVF
We know that one of the major factors contributing to in vitro fertilization failure is the high rate of chromosomal abnormalities in human embryos.
As women age the incidence of chromosomal abnormalities in mature eggs increases significantly. Studies have shown that starting in the early 30s, the rate of chromosomal abnormalities in human eggs (and therefore in human embryos) starts to increase significantly.
The rate continues to increase with advancing female age so that by the mid-40s a very high percentage of human embryos are chromosomally abnormal (over 75%).
It is believed that this is mainly due to problems with the spindle apparatus in the egg nucleus. The spindle is involved with properly lining up and segregating the chromosomes as the egg matures at the time of ovulation.
Older eggs have an inefficient spindle apparatus that does not line up the chromosome pairs properly and “mistakes” are made when splitting pairs of chromosomes. This leads to eggs that do not have the proper balance of 23 chromosomes – and will result in a chromosomally abnormal embryo if fertilized.
It has been shown that about 1% to 2% of human sperm are chromosomally abnormal on the average – as compared to about 20% to 90% of human eggs (depending on female age).
PGS – preimplantation genetic screening can be done on embryos prior to transfer to evaluate chromosomal competence.
Other genetic causes of implantation failure
- Implantation failure is probably sometimes caused by other genetic mutations – with a perfectly normal “karyotype” or chromosome complement
- There are tens of thousands of genes in the human genome – a lot of places where something can go wrong
- With time there will be genes discovered that are crucial for efficient embryo implantation – both on the embryo side and on the uterine side, and perhaps involving the immune system as well.