IVF embryo quality and day 3 embryo grading after in vitro fertilization
Cleavage Stage Embryo Grading
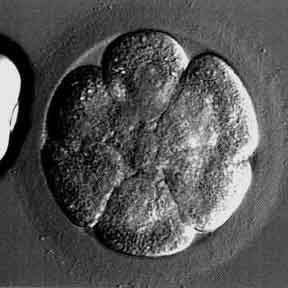
Embryo picture of a “perfect” looking 8-cell embryo (day 3 embryo)
There is no embryo fragmentation and the cells are very even, regular, and similarly sized
We call this is a “high quality” day 3 embryo
Embryo grading: 8 cell, grade 4
How is embryo quality assessment and grading done on day 3 of development?
There are many embryo grading systems that differ in how they assign grades and in whether a low number grade indicates the best or the worst embryo. We assess the “quality” of embryos from in vitro fertilization by carefully evaluating and scoring some aspects of their appearance.
Cell number
Embryos should be at 2 to 4 cells at 48 hours after egg retrieval and preferably about 7 to 10 cells by 72 hours. The cells in an embryo are also referred to as “blastomeres”.
Cell regularity – degree of regularity of size of blastomeres
It is generally best if the size of the individual cells (referred to as blastomeres) in the embryos are similar in size. If they are not, it is better if they are close to the same size, as compared to very different in size.
Degree of fragmentation
Fragmentation, also called blebbing, is a process where portions of the embryo’s cells have broken off and are now separate from the nucleated portion of the cell. It is preferable to have little or no fragmentation.
However, fragmentation in human embryos is quite common and many beautiful babies have resulted from the implantation of embryos with fragments. Many IVF labs, including ours estimates and records the percentage of fragmentation in each day 3 embryo. Embryos with more than 25% fragmentation have a low implantation potential.
Presence of multinucleation
An embryo is multinucleated if more than one nucleus can be seen in any individual cell on either day 2 or day 3. After day 3 it is extremely difficult to identify the presence of multinucleation. The great majority of multinucleated embryos have been shown to be chromosomally abnormal.
However, sometimes multinucleated embryos implant and lead to a healthy pregnancy and birth of a normal baby. These embryos are generally only transferred to the uterus if they are the only ones available.
Additional factors involved with embryo grading and selection for transfer
Other aspects of the microscopic appearance of the embryos are also noted including the presence of vacuoles, granularity, thickness of the outer shell (or zona pellucida), etc.
A slightly fragmented 8-cell embryo
Assisted hatching is being performed
The holding pipette is on the far left
A sperm is clearly visible at 7 o’clock (this sperm lost the race)
This embryo is high quality because it has an optimal cell number, the cells are fairly regular in size, and there is minimal fragmentation
Embryo grading: 8 cell, grade 3
This 5-cell embryo is moderately fragmented and has unevenly sized (irregular) cells
This embryo is expected to have a significantly lower chance of implanting because it is somewhat “slow” (more than 5 cells is preferred on day 3) and because of the significant fragmentation and irregularity of the cells
Embryo grading: 5 cell, grade 2
This embryo is severely fragmented and has unevenly sized cells
It is a poor quality day 3 embryo
This embryo probably does not have much chance to implant and make a viable pregnancy
Embryo grading: 6 cell, grade 1
Photo of a severely fragmented and very poor quality day 3 embryo
This embryo is essentially non-viable and is degenerating
It will not be able to continue normal development and implant
Embryo grading: 2 cell, grade 0
Multinucleated 2 cell embryo
Multiple nuclei (circular structures that look like moon craters) seen in both cells
This embryo does not have long term viability potential
Usually, determinations of “quality” are not made until at least 48 hours after the egg retrieval. However, some IVF labs have been carefully assessing embryos on the first day after egg retrieval at the zygote, or 1-cell embryo stage. They use morphologic parameters of the pronuclei on day one as part of the overall embryo quality assessment, and also as part of their selection criteria for the best embryos to transfer. This assessment on day one is an interesting tool, but it has not been shown to be consistently valid in different laboratories.
By 48 hours (“day 2”), the embryos must be to at least 2 cells – or they have “arrested”. We prefer that at least some of them are at the 3 or 4 cell stage by then.
By 72 hours (“day 3”), we like to see at least 6 cells – and preferably some at about 8 cells. We have seen babies that came from 4 cell embryos on day 3, but chances for pregnancy increase significantly with increasing cell number.
Embryos with higher cell numbers, regular appearing cells and little or no fragmentation have a higher overall chance of implanting than do other embryos with less cells, more irregularity and significant fragmentation.
Embryo quality as we see it under the microscope in the IVF lab gives us some reasonable ability to predict the chances for pregnancy after the embryo transfer procedure. However, because there are many other contributing factors involved that we can not see or measure, the generalizations about “quality” made from grading embryos are often inaccurate.
We see some cycles fail after transferring 3 perfect looking embryos, and we also see beautiful babies born after transferring only one “low grade” embryo. The true genetic potential of the embryo to continue normal development is very difficult to measure accurately unless we utilize preimplantation genetic screening (PGS) to select chromosomally normal embryos for transfer.
Chromosomal testing with PGS is done on several cells that are removed from expanded blastocyst stage embryos via trophectoderm biopsy. When PGS is done, the embryos are frozen after they are biopsied because the genetic testing results do not come back soon enough to do a fresh embryo transfer. In these cases we do a frozen embryo transfer about 4 weeks later.
- The rate of embryo implantation is substantially higher for embryos with normal PGS test results compared to unscreened embryos
- Therefore, to a great extent, true embryo quality is about chromosomal normalcy
- It is good for an embryo to get a high “grade” on morphology scoring
- However, being chromosomally normal is far more important in determining its destiny
An important variable that is often overlooked is the embryo transfer technique. A smooth transfer with no trauma to the endometrial lining is essential to give the embryos the best chance for implantation and continuation of normal development.
Ultimately, the true test of embryo quality is whether it implants and develops normally and eventually goes home from the hospital with mom and dad. In other words, embryo grading systems are imperfect, and we always need the pregnancy test, and the final pregnancy outcome, to tell us more about “embryo quality” than a microscope could ever reveal.
Most IVF clinics “grade” each embryo using one of many scoring systems. Unfortunately, there is no agreement at all as to which system to use. We all think we have the best one – and that the rest of the world should use our system – there are lots of big egos in the IVF world.
Patients often ask whether embryos that were given a “low grade” by the embryologist would result in a problem with the baby. As far as we know, the children born from low grade embryos are just as cute, intelligent, strong, etc. as those born from high grade embryos. The only difference seems to be with the chance for the embryo(s) to result in a pregnancy.
Embryo quality, to a great extent, is determined by the quality of the egg from which it started. Tests of ovarian reserve, such as the day 3 FSH hormone assessment, and antral follicle counts can give us useful information about egg quantity, but are not useful in predicting egg quality.
If we could improve the quality of the eggs that we start with in IVF, we would have a better chance of having a successful outcome. However, for the most part egg quality is predetermined and “we get what she gives”.
Egg quality is mostly determined by the chromosomal and genetic competence of the individual egg. There is no treatment to fix chromosomal or genetic defects. Therefore, we do our best with the eggs that we retrieve, or we screen blastocyst stage embryos for chromosomal status before transferring.
By getting numerous eggs, we have a better chance of having one or more with “high egg quality” – in other words, an egg that is fully competent and capable of fertilizing, developing normally, implanting and going on to become a healthy baby.
Learn how the number of eggs retrieved with IVF affects the chance for success
The quality of the ovarian stimulation process and the quality of the IVF laboratory itself are also very significant variables that impact the quality of the resulting embryos.