Embryo transfer procedure for in vitro fertilization – IVF Advanced Fertility Center of Chicago IVF embryo transfer technique and video
The embryo transfer procedure is the last one of the in vitro fertilization process. It is a critically important procedure. No matter how good the IVF laboratory culture environment is, the physician can ruin everything with a carelessly performed embryo transfer. The entire IVF cycle depends on delicate placement of the embryos at the proper location near the middle of the endometrial cavity – with minimal trauma and manipulation.
- The importance of proper embryo transfer technique for successful IVF cannot be overstated
- Ultrasound guided embryo transfer is the most efficient technique currently available
For IVF, the woman is stimulated with injectable medications to develop multiple eggs. Eggs develop in follicles in the ovaries. When the follicles are mature, the egg retrieval procedure removes eggs from the ovaries. Sperm is added to the eggs and the next day we check the eggs for evidence of fertilization. An appropriate number of embryos are transferred to the uterus several days later – using ultrasound guidance for best placement.
Click “play” to see a 30 second embryo transfer video
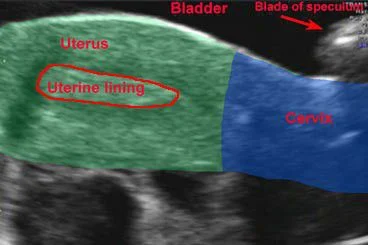
Uterus colored to explain embryo transfer video
Same view of uterus as in embryo transfer video above
Uterus shaded green, cervix in blue
Target for embryo transfer placement is the middle of the lining
Ultrasound guided embryo transfer technique
The embryo transfer procedure seems very similar to a Pap smear for the woman. There should be no pain and no sedation or other drugs are required. We use a moderately full bladder for embryo transfer. This helps in 2 important ways. It allows good ultrasound visualization of the catheter which helps with smooth and proper transfer of the embryos to the best location, and it also unfolds the (anteverted, “tipped up”) uterus to a more accommodating angle,making the process smoother and less traumatic for the uterine lining and the embryos.
The embryo transfer catheter is loaded (see video of this) with the embryos and the physician passes it through the cervical opening up to the middle of the uterine cavity. Abdominal ultrasound is used simultaneously to watch the catheter tip advance to the proper location. It is sometimes difficult to keep the tip of the catheter in the exact plane of the ultrasound beam at all times – but it is very important to control the proper placement of the embryos (see the video above).
When the catheter tip reaches the ideal location, the embryos are then “transferred” (squirted out of the catheter) to the lining of the uterine cavity (endometrial lining) by the infertility specialist physician. After the embryos are transferred, the catheter is slowly withdrawn and checked under a microscope for any retained embryos. If an embryo is retained in the catheter (uncommon) the transfer procedure is repeated immediately and the catheter is checked again.
Proper location for placement of the embryos at transfer
Research has been done to determine the optimal location to place the embryos in the uterine cavity. Basically, the middle of the endometrial cavity – half way from the internal os of the cervix to the uterine fundus (top of cavity) – is the best place. Care should be taken to keep the catheter between the top and bottom layers of the endometrium and not to allow it to dissect under the endometrial surface. This is called subendometrial embryo transfer. Pregnancies will occur with subendometrial placement of the embryos, but success rates are lower.
Smooth, efficient and effective embryo transfer
Best with a moderately full bladder for good ultrasound visualization and a better angle
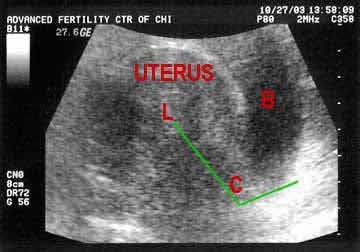
embryo transfer empty bladder
Poor quality ultrasound image of uterus – empty bladder
The uterus and lining have a very fuzzy appearance. There is also a severe angle between the cervix and uterus (angle indicated by green lines). This woman drank water to fill the bladder before the transfer. With the full bladder, the angle in the cervix was reduced and the uterine lining was clear.
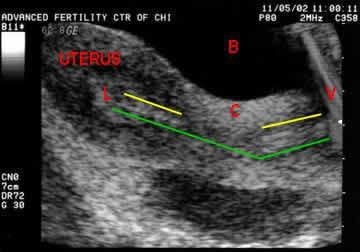
Ultrasound for ivf embryo transfer
Excellent ultrasound image at embryo transfer – full bladder
During the embryo transfer procedure the Wallace catheter is seen in the cervix and uterine lining (below the yellow lines). The embryos are released from the catheter tip – at “L”. Minimal angle between the cervix and uterus (green line).
Cervix = C, Bladder = B, Lining = L, Vagina = V
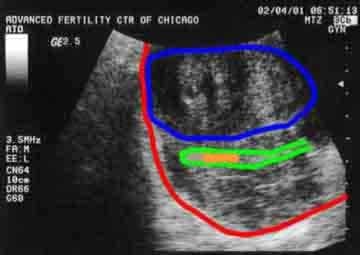
Difficult embryo transfer
Difficult ET
The uterus is sometimes a little “tricky”. Here it is distorted by myomas (fibroids), making the embryo transfer itself – and visualization with ultrasound difficult.
Embryo transfer with fibroids
Same image: Uterus outlined in red, myoma in blue, endometrial lining outlined in green. Catheter needs to place embryos between green lines – in the orange area.
Activity restrictions and bed rest after IVF transfer
At our IVF clinic, we have the woman lie on her back for 1 hour after embryo transfer before going home. We request that she also limit physical activity for the remainder of that day. This means bed rest after the IVF transfer for the rest of the day and that night. It does not necessarily mean total “bed rest” but can be hanging out on the couch or in the Lazy-boy recliner – watching videos, reading, bossing hubby around, etc.
We allow “normal activity” such as working, walking around, etc. beginning the morning after the embryo transfer. Heavy bouncing of the uterus is restricted until after the pregnancy test. Therefore, water skiing, jogging, “uterus bouncing sex”, and other high impact activities are probably not a good idea until after the pregnancy test. Once pregnant, we should be OK to start all that fun stuff again.
IVF embryo transfer and travel
For our couples that travel here from out of town for IVF and embryo transfer, we recommend that they do not fly out on the day of the transfer, but wait until the next day. For patients that are diving back home – it is acceptable to drive home (regardless of the length of the drive) after one hour of bedrest in our office following the transfer procedure.
Come here from out of town to do IVF
When does the embryo implant following IVF transfer?
A healthy human embryo will hatch from its shell on day 5-7 after fertilization and implant within hours after hatching out. So actual invasion of the embryo with attachment to the uterine wall occurs about 2-5 days after a day 3 transfer and within 1-3 days after a day 5 transfer.
How soon to do a pregnancy test after IVF?
About 9-11 days after the transfer (9 days for day 5 transfer and 11 days for day 3 transfer), we do a blood test to find out if she is pregnant. If embryo implantation has occurred, HCG hormone will be detectable in the mother’s blood at that time.
We don’t recommend doing a urine pregnancy test (HPT) after IVF. The reason is that there are a lot of falsely negative results. We have seen many beautiful babies born after the female partner called us to say that she took a home urine pregnancy test that was negative. A blood test is needed because it is much more sensitive and reliable.
How many embryos can be implanted in IVF?
At our IVF clinic, the number of embryos to be transferred is decided by the couple after a discussion with the physician regarding their embryo quality and how it impacts on the risks for multiple pregnancy versus the risk of failing to conceive at all. As female age increases, the implantation rate of the embryos tends to decline. This means that the chance that an embryo will implant drops gradually (and progressively) as the female partner ages beyond about 32 years old.
On the baby side of things, a singleton pregnancy is safest. So, in general, we would prefer that only one fetus actually implants and continues development. However, because couples fear failing IVF more than they fear the risks of twins, the majority decide to replace back 2 embryos when the female partner is under 38, 2 or 3 embryos when she is 38-40, and 3 or 4 (if they have that many) if she is 41 years old or more. Transferring this number of embryos seems to result in a “reasonable” balance of high overall pregnancy success rates, and low rates of high-order multiple (triplets or more).
Our IVF pregnancy success rates
Learn about blastocyst transfer an IVF technique with high success rates