We have been doing day 5 blastocyst transfer since 1998 at the Advanced Fertility Center of Chicago, IL.
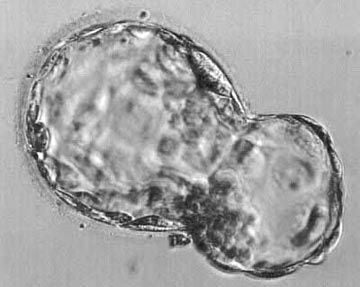
Blastocyst hatching from its shell – at lower right
After hatching, the embryo implants in the uterus lining
Photo just before embryo transfer procedure
Balance risks and benefits with IVF
Couples with infertility often express a desire for delivering twins instead of a single child. They may think; “we want kids, and all this treatment is expensive and unpleasant, so let’s just have 2 kids and get it over with”.
When they are fully aware of the risks to the children if delivery is premature, some couples no longer prefer a multiple pregnancy. However, after full disclosure of the risks, many couples still hope for twins. Of course, they are also hoping that their children will be perfectly healthy.
The psychological, social, and economic stresses involved with caring for twins is substantial, but patients often say they would welcome facing those stresses if they were so blessed.
The risks of a multiple pregnancy are high. These expectant mothers face an increased risk for developing complications of pregnancy such as gestational diabetes, pre-eclampsia, preterm labor, hemorrhage, and other complications. The risks to the fetuses and children are mostly related to premature delivery and can be very severe.
Compared to a singleton, a twin is about five times more likely to die in the first year of life. For a triplet, this risk is about 13 times that of a singleton. The risk of having a lifelong handicap (e.g., cerebral palsy, mental retardation) is increased about 10 times for twins compared to singles, and these risks are substantially higher for triplets. Quadruplet and other high-order pregnancies are much riskier. Fortunately, with current embryo transfer policies, pregnancies beyond triplets are rare with IVF.
Statistics about the number of embryos transferred and multiple pregnancies
- These reports cover live birth rates, twin and triplet rates, the average number of embryos transferred per patient and other variables
The report for IVF cycles in 2015 is currently available on the SART website, the CDC report lags behind the SART report – 2015 preliminary data is the most recent available from CDC.
These annual reports show the trend in the United States toward transferring fewer embryos.
- In 1997, the average number of embryos transferred to women under 35 was 3.7
- By 2000, it was down to 2.9
- Over the same time period, there was a significant increase in the overall live birth rates for IVF procedures
- At the same time, the percentage of births that were triplets or more dropped from about 14% to about 9%
- However, over the same period of time, no progress was made with regard to reducing the rate of twin pregnancies, which remained at about 32% of births.
- Over that 4-year period, US IVF centers transferred less embryos, resulting in higher success rates, a lower percentage of triplets, but no change in the percentage of twins.
In general, European infertility clinics are transferring fewer embryos as compared to American IVF centers. On average, they have lower pregnancy rates and a lower percentage of multiple births than clinics in the United States.
There are several factors involved in this difference. In some European countries, physicians are restricted by law so that they cannot transfer more than two embryos. Also, IVF is more commonly paid for by insurance or socialized medical systems in Europe.
In the United States, couples with insurance coverage for IVF services are more likely to prefer fewer embryos for transfer. By comparison, couples who must pay out of pocket for IVF often request that more embryos be transferred. They tend to be fearful of failure because of the high financial costs associated with repeating the IVF process.
What is the appropriate number of embryos to transfer?
In 2017, the American Society for Reproductive Medicine (ASRM) and SART published revised guidelines regarding the appropriate maximum number of embryos to transfer. The ASRM guidelines suggest a maximum number of embryos to transfer based on the day of transfer (cleavage stage vs. blast), “prognosis category” (favorable vs. all others), whether preimplantation genetic screening was done to screen out chromosomally abnormal embryos, and female age.
Current ASRM – SART guidelines on maximum number of embryos to transfer (updated 2017)
| Maximum Number of Embryos to Transfer | ||||
|---|---|---|---|---|
| Age < 35 | Age 35-37 | Age 38-40 | Age 41-42 | |
| Favorable Prognosis | 1 | 1 | 3 | 4 |
| All others | 2 | 3 | 4 | 5 |
| Euploid | 1 | 1 | 1 | 1 |
| Maximum Number of Embryos to Transfer | ||||
|---|---|---|---|---|
| Age < 35 | Age 35-37 | Age 38-40 | Age 41-42 | |
| Favorable Prognosis | 1 | 1 | 2 | 3 |
| All others | 2 | 2 | 3 | 3 |
| Euploid | 1 | 1 | 1 | 1 |
The ASRM identifies the following characteristics as being associated with a “more favorable prognosis”:
- First cycle of IVF
- Good embryo quality by morphology grading criteria
- Excess embryos available for freezing
- Having a previous successful IVF cycle
These guidelines have been helpful in limiting the number of embryos transferred, particularly in patients with the most favorable prognosis. However, many couples in the other categories who choose to have more than two transferred could still be at high risk for multiples, including triplets. Also, patients with embryos that have a high potential for implantation might have a high risk of twins if they have two transferred.
Couples with a very high chance for pregnancy can be identified on the day of embryo transfer and can be offered the option of transferring one or two embryos.
When a couple has high-quality embryos available for transfer on day 5 and they are offered the options of transferring one embryo with a 50% expectation for pregnancy (almost all singles) or two embryos with an 75% expectation for pregnancy (about 38% twins, 60% single, and 2% triplets), most couples choose to transfer two embryos. This is after counseling them about the medical risks involved for mother and babies with multiple pregnancies.
They want the higher chance for pregnancy and are accepting (sometimes even welcoming) the risks that are involved with a multiple pregnancy. Those who choose to have a single embryo transferred usually have insurance coverage for IVF or have at least one child already.
What is blastocyst culture and transfer?
In past years, the majority of embryo transfers were done on day 3 (after the egg retrieval) at the “cleavage stage” when the embryos have four to eight cells. One problem with this is that day 3 embryos normally are found in the fallopian tubes, not in the uterus. The embryo first moves into the uterus at about 80 hours after ovulation. The embryo implantation process begins about 3 days later, after blastocyst formation and hatching have occurred.
The other problem with transferring on day 3 is that many embryos at that stage do not have the capacity to continue development and become high-quality blastocysts. We do not have reliable methods to determine which of the day 3 embryos will be viable long-term. Therefore, the tendency has been to transfer more embryos on day 3 in an attempt to achieve good pregnancy rates.
When embryos are cultured from day 3 to day 5, some will stop developing and others (usually 25% to 60%) will continue to become blastocysts. Therefore, by choosing the best blastocysts for transfer on day 5, we can choose much more reliably those with the best potential for implanting and making a baby.
In the past it was difficult to get good numbers of high-quality blastocysts with in vitro culture systems. However, advanced culture media have been developed that provide the proper balance of nutrients at the various stages of early embryo development. Proper culture techniques with these new media formulations yield excellent blastocyst formation rates. This makes blastocyst transfer a viable option for some couples with infertility.
Some programs are doing all IVF cases with day 5 transfers. One of the issues with this is that a small proportion of couples will have embryos that are growing on day 3, but by day 5, all of their embryos have stopped developing. These patients could have had a day 3 embryo transfer, but because their embryos were kept in culture and arrested after day 3, they will not have an embryo transfer at all. This has been reported to occur in about 5% of cases if all patient’s embryos are cultured for 5 days.
The ultimate outcome of the cycle might be exactly the same either way (a failed cycle), but many couples would prefer to have an embryo transfer and then not be pregnant as opposed to being called and told that their embryos have stopped developing and therefore they will not have an embryo transfer procedure.
Our IVF program and many others perform blastocyst transfers in selected cases. Most IVF centers (including ours) that perform day 5 transfers have selection criteria for deciding which cases are transferred on day 3 versus day 5. The criteria often involve a minimum number of fertilized eggs or a minimum number of embryos that are still developing on day 3.
In our IVF program, we (currently – 2017) usually perform day 3 transfers for couples (female age under 37) with less than 3 day 3 embryos, and do day 5 transfers for couples with 3 or more day 3 embryos. This has been working well for us with rare cases having no embryos available for transfer on day 5. Individual factors are often important in making this decision, such as:
- Age of the female partner
- Information from previous IVF cycles
- The planned number of embryos to be transferred to the uterus (1, 2 or 3)
- Whether preimplantation genetic screening is desired by the couple
Do blastocyst transfers correlate with higher pregnancy rates than day 3 transfers?
Yes, in most published studies, and in the experience of many IVF programs, pregnancy rates are higher with blastocyst transfers when a given number of embryos are transferred (e.g. two). This is because of the higher potential for implantation of the blastocyst.
However, the issue is complicated because some IVF centers have seen no improvement or even lower pregnancy rates with blastocyst transfers. This is because blastocyst culture and transfer is technically more complicated and difficult as compared to day 3 transfer. Some laboratories are not able to maintain the stable and exacting culture environment for 5 days that allows the optimal development of the embryos.
Therefore, it is not surprising that extended culture and transfer of two embryos on day 5 can show excellent pregnancy rates in some centers and significantly lower results in others. This concept is well-understood in the embryology world, but it is not widely discussed in public forums.
How can blastocyst transfer benefit couples needing IVF?
Transferring only two embryos on day 3 results (on average) in an even lower rate of twin and triplet pregnancies (a good thing), but this happens at the cost of a lower overall pregnancy rate.
Because of the high implantation potential of blastocyst embryos, we should be cautious about the high potential for twins. Transfer of two good looking blastocysts can result in twin pregnancy rates as high as 50%. Therefore, transferring only one should be considered in young women (or in egg donation cycles) with high-quality blastocysts.
Pregnancy rates with single embryo transfer (SET) in these patients can be in the 40-60% range in good IVF programs with a very low risk of twins (about 2% due to embryo splitting – identical twins).
How can PGS testing benefit couples needing IVF?
When we screen embryos prior to the transfer with preimplantation genetic screening (PGS) we see excellent pregnancy and live birth success rates after transfer of a single embryo when it has normal PGS results. We now have years of experience with doing this for couples that choose to have it.
Conclusions
- Blastocyst culture and transfer of one or two embryos in IVF centers that are proficient with this technique currently offers the best balance between the chances of having any pregnancy and the risks of multiple pregnancy.
- The decision to transfer one or 2 (or more) should be based on the age of the female, the morphology grading of the blastocysts and the history of their previous IVF treatments.
- Doing PGS screening on blastocysts and then transferring a single embryo is currently the state of the art for IVF. It provides a high probability for a healthy outcome for mother and baby and reduces miscarriage risk.
Cost of blastocyst transfer
We are not currently charging extra for blastocyst transfer.