High AMH Levels in Women Under Age 35 Undergoing IVF Are Correlated With High Live Birth Rates. Women With Very Low AMH Levels Have High Cancellation Rates but Reasonable Live Birth Rates.
Research study presented by Richard Sherbahn, MD at the 69th Annual Meeting of the American Society for Reproductive Medicine, Boston, MA, October, 2013.
What is AMH and why should we care about it?
- AMH, anti-mullerian hormone, is made by follicles in the ovaries
- It is one of the tests used to measure ovarian reserve - egg supply
- Female age is primary determinant of live birth with IVF
- At a given age, women with higher ovarian reserve do better with IVF
- AMH can be used to predict a woman's response to IVF stimulation drugs and to predict IVF success rates
- It can be used to adjust the stimulation protocol prior to starting IVF
Ovarian Reserve and Age and IVF Success
- As women get older and egg quality declines, the need for embryo selection becomes more important
- Fertility docs sometimes will exclude patients with low AMH from IVF treatment with the assumption that chances for success are too low
- However, this denies treatment to couples with low or possibly moderate success rates
AMH and Prediction of IVF Outcome
- Published studies generally say that age and AMH are independently associated with live birth
- Nelson et al., 2007; Gleicher et al., 2010; La Marca et al., 2010; Majumder et al., 2010
- The primary relationship is supposed to be with egg yield
- Nelson et al., 2007; Majumder et al., 2010
- However, some authors say AMH also gives information about egg quality
- Brodin, et al., J Clin Endocrinol Metab, 2013
Study Objective
The objective of this study was to determine how well serum AMH levels in women under 35 predict IVF outcome
Study Design and Methods
- Retrospective chart review
- October 2008 to December 2012
- All 786 cycles in women under 35 stimulated for IVF using own eggs with known AMH levels
- Cycles with all embryos frozen for PGD or PGS were excluded
- Beckman Coulter AMH Gen I or Gen 2 ELISA AMH assays
- Patients were placed in 3 groups based on their serum AMH level
- Low group had <0.6 ng/ml
- Middle group had 0.6-1.5 ng/ml
- High group had >1.5 ng/ml
Outcome parameters assessed
- IVF cancellation rate per cycle
- Average number of eggs retrieved
- Live birth rates per cycle
IVF Results For 3 AMH Groups
| AMH Level (ng/ml) |
# of Cycles | Cancellation Rate | Mean # Eggs | Live Birth Rate Per Cycle |
|---|---|---|---|---|
| <0.6 Low Group |
53 | 15.1% | 7.0 | 43.4% |
| 0.6-1.5 Middle Group |
188 | 3.7% | 9.3 | 43.6% |
| >1.5 High Group |
545 | 0.4% | 14.2 | 63.9% |
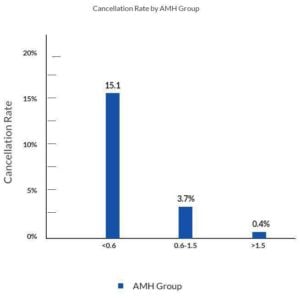
Cancellation rate by AMH
IVF cycle cancellation rate is much higher with low AMH levels
Differences between all groups are statistically significant
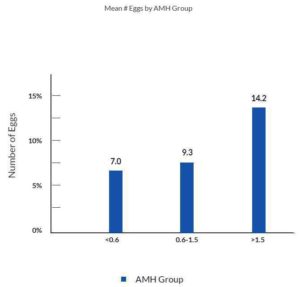
Number of eggs by AMH level
Average number of eggs retrieved is lower with low AMH levels
Differences between all groups are statistically significant
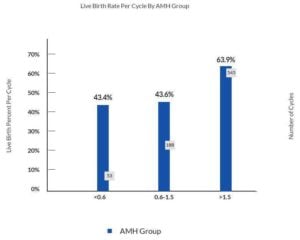
Live birth success rate by AMH level
Live birth success rates are lower with low AMH levels
Low and middle groups are significantly lower as compared to the high group
Why do our results differ from other studies and why are our live birth rates so high in the low AMH group?
In this study, the low AMH group has a large range of antral follicle counts. The average antral count was 11.2, with a standard deviation of 5.1and a range of 2 to 26. The antral follicle count is known to be a good predictor of response to stimulation and IVF success rates. This large range of antral follicle counts in the lowest AMH group suggests that AMH levels might not accurately and reliably predict ovarian reserve.
- It is possible that women under 35 are different regarding low AMH levels and prediction of IVF success
- The aggressive IVF stimulation and augmentation protocols that we use for patients with low ovarian reserve might account for the high success rates.
Conclusions
- High AMH levels correlate with low cancellation rates, retrieval of more eggs, higher live birth rates and a high chance for cryopreservation.
- Couples should not be excluded from attempting IVF due to low AMH values alone because the live birth rates were reasonable.
- At our center, low AMH levels do not predict low IVF success rates in women under 35.
Categories
About the AFCC Blog
Welcome to the Advanced Fertility Center of Chicago’s blog! Here, you will find information on the latest advancements in fertility care and treatments, including IVF, IUI, third-party reproduction, LGBTQ+ family building, preimplantation genetic testing, and more. Since 1997, we’ve used our experience and continuous investment in the latest fertility technology to help thousands of patients grow their families. Contact us today for more information or to schedule a new patient appointment.