Uterine problems can cause infertility or miscarriage. A (fairly) normal uterine cavity and endometrial lining are necessary in order to conceive and maintain a pregnancy.
There are several conditions related to the cavity or the lining that can cause problems.
- When a woman has her menses (period) the endometrial lining of the uterus and some associated blood is shed. Then a new lining is regenerated over the next few weeks or so and eventually becomes receptive to implantation of an embryo.
- If no embryo implants, her body recognizes that she is not pregnant and it sheds the uterine lining and starts the regeneration process over again.
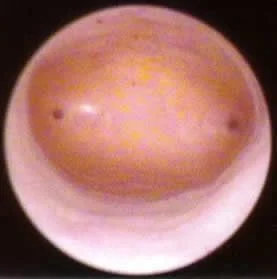
Hysteroscopic view of inside a normal uterine cavity.
Office hysteroscopy – we are looking up from the cervix at the top of the uterine cavity.
The tubal ostia (openings of fallopian tubes into uterus) are the dark spots at 3 and 9 o’clock.
Ultrasound images of a uterus with a normal endometrial lining thickness of 11 mm
Same image showing the outer contour of the uterus outlined in red and the “triple stripe” endometrial (uterine) lining outlined green. Cervical canal is well visualized at lower right.
Problems of the uterus and uterine lining that can cause or contribute to reproductive problems such as infertility or recurrent miscarriage:
- Uterine Polyps
- Uterine Fibroids (proper medical terminology is myoma or leiomyoma)
- Intrauterine adhesions – scar tissue within the uterine cavity, also called Asherman’s Syndrome. This can interfere with conception, or can increase the risk of a miscarriage.
- Congenital uterine malformations, such as a bicornuate uterus, a T-shaped uterus, or a uterine septum
- Luteal phase defect – an uncommon condition that involves inadequate development of the microscopic and cellular changes in the endometrial lining of the uterus after ovulation and exposure to the hormone progesterone.
- Thin endometrial lining – this is also uncommon. We like to see a lining of at least 8mm in thickness when measured by ultrasound at the time of maximal thickness during the cycle (see above ultrasound picture of an 11.2 mm lining).
There is some debate about “how thin is too thin”, as well as to “how thick is too thick”.
- In general, 8-13 mm is good, less than 6 is potentially a problem, and greater than 15 or so might possibly reduce chances for successful pregnancy.
During IVF treatment, the uterine lining starts at about 3mm thick at the end of the menstrual period. After estrogen levels rise sufficiently, the lining of the uterus thickens by about 1mm each day during IVF.
Hysteroscopy is a surgical procedure that involves insertion of a narrow telescope-like instrument through the vagina and cervix into the cavity of the uterus (endometrial cavity). The cavity is then distended with fluid (such as salt water) and can be visualized through the scope. This procedure allows us to see any defects inside the cavity.
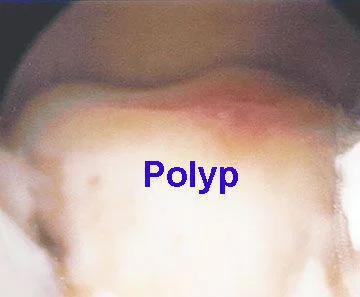
Uterine polyp seen by hysteroscopy
Large uterine polyp on the “floor” of the uterine cavity – seen with hysteroscopy
Ultrasound is a very useful tool for evaluating the pelvis and the uterus and its lining, or endometrium. 3D ultrasound, a newer technology, is particularly good at helping doctors to characterize the shape of the uterine cavity.
Normal uterine configuration vs. uterine septum
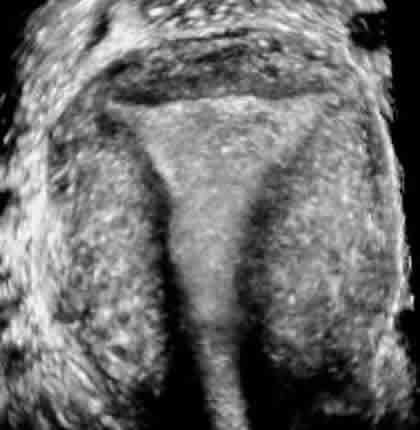
Ultrasound of a normal uterus in the coronal plane
The endometrial cavity has a smooth triangular shape
Cervix is at the bottom of the image
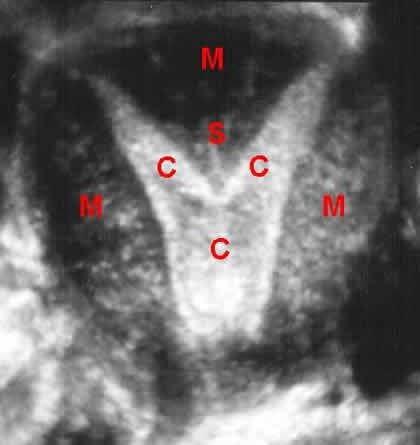
A uterine septum on a coronal plane from 3D ultrasound
Endometrial lining and uterine cavity = C
Muscle part of uterus = M
Septum “pushing down” into cavity = S
A septum is like extra muscle “pushing down” from the top into the cavity
This ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at “C”) only goes to one fallopian tube (goes up to her right tube)
The other side of the uterus and the left tube are congenitally absent
Congenital uterine abnormalities such as a unicornuate, septate or bicornuate uterus can cause reproductive problems such as miscarriage, preterm labor and preterm birth.
Office hysteroscopy image of a uterine septum looking up from cervix towards top of uterus
Septum dividing the cavity at “S”
The left side of her uterine cavity is at “L”, the right side is at “R”