Varicoceles in Men and Infertility
When Should Surgery Be Done?
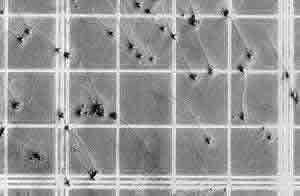
Numerous sperm - at high magnification on a counting chamber
About 25% of all infertility cases are caused by a sperm defect, and 40-50% of infertility cases have a sperm defect as the main cause or a contributing cause. This is known as male factor infertility.
A varicocele is an abnormal dilation of veins within the spermatic cord, similar to a varicose vein in the scrotum. It can potentially affect sperm by increasing testicular temperature, which may impact sperm quality.
- 40% of infertile men
- 20% of all men in the general population, the majority of whom are fertile with normal sperm
Urologists often diagnose and surgically repair varicoceles. However, correcting a varicocele does not always improve semen quality enough to change the required therapy for conception. Several studies have shown that while varicocele surgery may improve sperm counts or motility, randomized trials do not consistently show improved pregnancy rates. Thus, if a couple requires inseminations or IVF anyway, varicocele surgery may not be beneficial.
For example, if the sperm count is below 5 million per cc or motility is under 30%, it is unlikely that surgery will improve semen quality enough for natural conception. In such cases, IVF with ICSI may be necessary. Men with slightly low sperm counts (15-20 million) may be better candidates for varicocele surgery, although couples with these sperm parameters often conceive on their own. However, if the female partner has blocked tubes or an ovarian reserve issue, male surgery may not be indicated.
There are six controlled, randomized published trials of varicocele surgery vs. no surgery:
- 3 studies showed lower pregnancy rates with surgery
- 3 studies showed higher pregnancy rates with surgery
- A meta-analysis of these six studies found no significant effect of surgery on pregnancy rates
The effectiveness of varicocele surgery as a treatment for male infertility remains uncertain.
- Couples considering varicocele surgery should consult both a trained urologist and an infertility specialist to understand all available options.
- Some couples (especially those with a young female partner) may choose to try surgery and see the outcome.
- Varicocele surgery is not highly invasive, and recovery is relatively easy. If conception does not occur within 6-12 months post-surgery, other options like insemination or IVF with ICSI remain available.
Categories
About the AFCC Blog
Welcome to the Advanced Fertility Center of Chicago’s blog! Here, you will find information on the latest advancements in fertility care and treatments, including IVF, IUI, third-party reproduction, LGBTQ+ family building, preimplantation genetic testing, and more. Since 1997, we’ve used our experience and continuous investment in the latest fertility technology to help thousands of patients grow their families. Contact us today for more information or to schedule a new patient appointment.