PESA and TESA Sperm Aspiration and ICSI vs. Vasectomy Reversal Surgery
Costs and Success Rates of Fertility Options after Vasectomy
Many men who have had a vasectomy for contraception may later wish to have children again, often due to changes in personal circumstances. There are three general options to consider for further childbearing in this situation:
- Vasectomy reversal surgery.
- Sperm aspiration from the testicle or vas deferens, followed by ICSI, IVF, and embryo transfer.
- Donor sperm insemination of the female partner.
Sperm can be aspirated from the testicle or the vas deferens (near the testicle) with minimal discomfort. This procedure, known as PESA or TESA, is performed under local anesthesia and typically takes about 30 minutes.
- PESA: Percutaneous Epididymal Sperm Aspiration
- TESA: Testicular Sperm Aspiration
- TESE: Testicular Sperm Extraction (requires a small incision, often performed in a hospital)
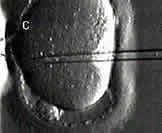
Photo of ICSI in progress: ICSI needle inside egg, sperm being injected
Sperm can be used fresh or frozen for future IVF attempts. Generally, a urologist specializing in male fertility will perform the aspiration, but in some cases, it may be done by a reproductive endocrinologist.
Costs range from $3,000 to $12,000 depending on various factors, including the location (office vs. hospital) and the type of anesthesia. Currently, AFCC charges $3,300 for sperm aspiration performed in-office, which includes urologist fees, facility fees, sperm freezing, and six months of storage.
The cost of ICSI at AFCC is $1,500, and IVF is $10,000. This includes ovarian stimulation monitoring, all IVF procedures, and anesthesia. More details on pricing plans can be found on our IVF costs and pricing page.
Success depends largely on the IVF lab's live birth rates and the age of the female partner. We generally expect similar or slightly higher success rates compared to other couples undergoing IVF with female partners of the same age. The female partner's ovarian reserve, measured by antral follicle count, is a good predictor of success.
Vasectomy reversals are more successful if performed within 10 years of the initial procedure, after which success rates decline. The surgery typically costs $10,000 to $15,000 and is performed by a urologist.
- Advantages: If successful, no further medical assistance is needed for future pregnancies.
- Disadvantages: High cost and possible need for additional birth control or sterilization if only one more child is desired.
Donor sperm insemination is a straightforward process in which frozen donor sperm is thawed and placed in the uterus at ovulation time. Couples can select a donor from a certified sperm bank.
Vasectomy reversal may be the best initial option for couples with a relatively young female partner and a recent vasectomy. For females over 35, a fertility evaluation should precede any procedure. If reversal surgery is unsuccessful, sperm aspiration with IVF-ICSI may be more effective.
- It’s often beneficial to consult both a reproductive endocrinologist and a urologist.
- General urologists may not be familiar with IVF-ICSI, and reproductive endocrinologists do not perform vasectomy reversals, so a team approach may be ideal.
Categories
About the AFCC Blog
Welcome to the Advanced Fertility Center of Chicago’s blog! Here, you will find information on the latest advancements in fertility care and treatments, including IVF, IUI, third-party reproduction, LGBTQ+ family building, preimplantation genetic testing, and more. Since 1997, we’ve used our experience and continuous investment in the latest fertility technology to help thousands of patients grow their families. Contact us today for more information or to schedule a new patient appointment.